Introduction
In the vast landscape of medicine, antibiotics stand as a monumental achievement, reshaping the narrative of bacterial infections and making profound contributions to global public health. Rooted in the Greek words “anti” and “bios,” meaning against and life, respectively, antibiotics form a diverse family of medications engineered to hinder bacterial growth or eradicate these microscopic foes. Sir Alexander Fleming’s discovery of the first antibiotic, penicillin, in 1928, etched an indelible mark in medical history, heralding a new epoch in the management of infectious diseases.
The Marvel of Antibiotics:
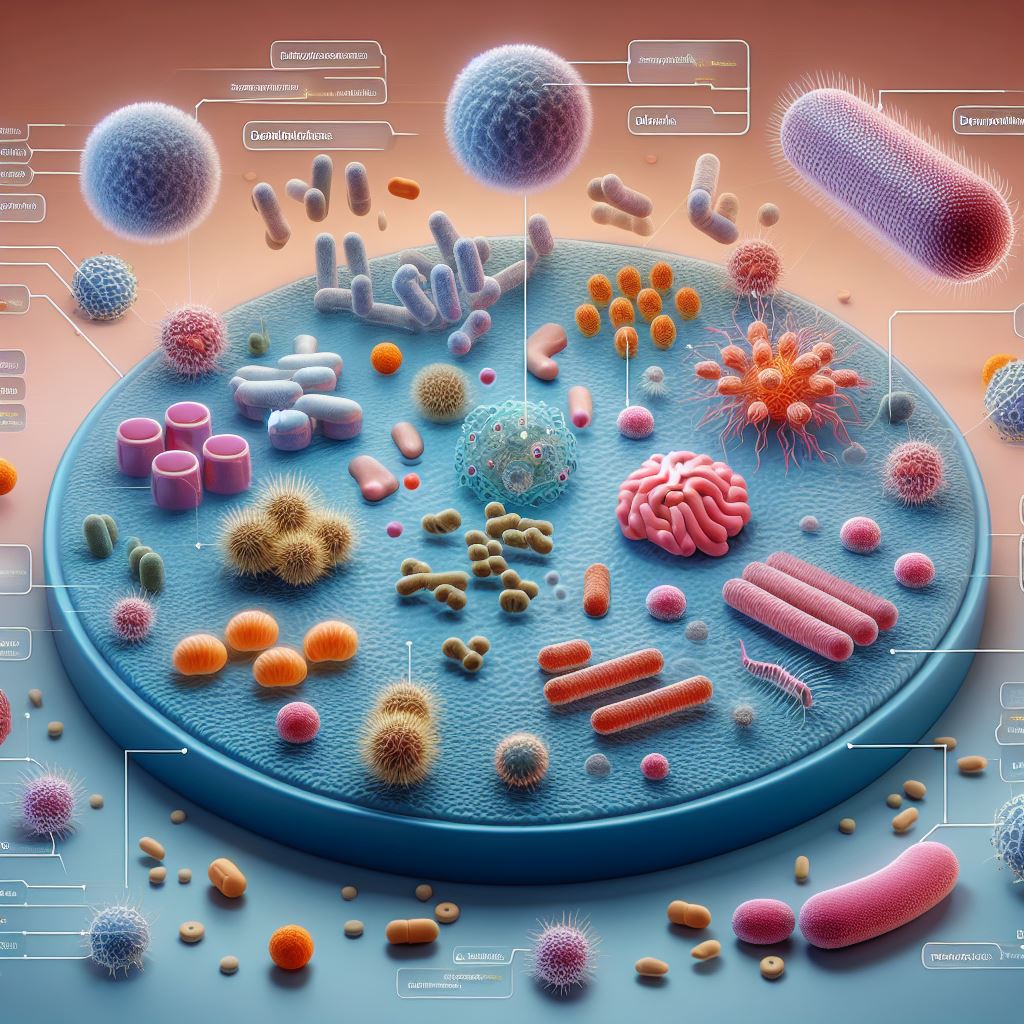
These extraordinary compounds operate by honing in on specific bacterial structures or processes, disrupting their ability to flourish and propagate. Over time, scientists have meticulously crafted an expansive arsenal of antibiotics, each endowed with distinctive mechanisms of action. This rich variety effectively treats a broad spectrum of bacterial infections, offering a lifeline to countless individuals facing microbial adversaries.
Navigating the Complexity:
Yet, the story of antibiotics is not without its challenges. The overzealous use and abuse of these powerful agents have given rise to a formidable foe – antibiotic-resistant strains of bacteria. This global health menace threatens to undermine the efficacy of our most potent weapons against infections.
The Call for Balance:
As we embark on a journey through the intricate terrain of antimicrobial agents, we must strike a delicate equilibrium. This involves not only embracing the life-saving potential of antibiotics but also vigilantly safeguarding their efficacy for the well-being of present and future generations. To comprehend the full tapestry of antibiotics, one must delve into their mechanisms, explore their diverse types, and appreciate the historical milestones that have shaped their evolution.
1. Can you drink alcohol while taking antibiotics?

2. Do antibiotics make you feel tired?

3. How long does it take for antibiotics to work?
4. Do antibiotics harm your body?
| Read more: Air Pollution – What Causes Air Pollution? |
| The healthy-life-expert.com crew collected the information via a field visit to provide accurate and genuine information. |