Table of Contents
ToggleIntroduction
Cancer is a formidable adversary, a diverse group of diseases characterized by the uncontrollable growth and division of abnormal cells. Its pervasive reach extends across the globe, making it a leading cause of morbidity and mortality. The quest to combat this complex ailment hinges on recognizing its elusive symptoms and understanding the intricate web of factors contributing to its development, facilitating early detection, diagnosis, and effective treatment.
Symptoms of Cancer:
The manifestations of cancer are as varied as the diseases themselves, contingent on the type, location, and stage of development. Nevertheless, certain telltale signs should not escape our attention:
✔. Unexplained Weight Loss: The abrupt and unexplained shedding of pounds, especially when it transpires swiftly, may serve as a red flag for various cancers. Cancer cells’ voracious appetite can deplete the body’s energy reserves, resulting in weight loss.
✔. Persistent Fatigue: A relentless and unrelieved fatigue that persists despite rest should not be dismissed lightly. Cancer-related fatigue, often incapacitating, can cast a shadow over daily activities and warrant thorough investigation.
✔. Changes in Skin or Moles: Alterations in the color, size, or shape of moles, or the emergence of new skin irregularities, merit scrutiny by healthcare professionals. Such changes may hint at underlying skin cancers demanding attention.
✔. Persistent Pain: Unexplained and enduring pain, particularly when confined to a specific area, may serve as a harbinger of cancer. Identifying the source of such pain through meticulous medical evaluation is imperative.
✔. Changes in Bowel or Bladder Habits: Disruptions in bowel habits, be it persistent diarrhea or constipation, alongside changes in bladder function, could signify colorectal or bladder cancers, respectively.
✔. Difficulty Swallowing or Persistent Indigestion: The struggle to swallow or enduring indigestion may be indicative of gastrointestinal cancers, such as esophageal or stomach cancer.
✔. Cough or Hoarseness: A lingering cough or persistent hoarseness that defies resolution over time may raise suspicions of lung or throat cancer.
Causes of Cancer:
The genesis of cancer is intricate, often entwining genetic predispositions, environmental exposures, and lifestyle choices. The following factors contribute to this intricate tapestry:
✔. Genetic Factors: Specific genetic mutations inherited from parents can elevate the risk of developing certain cancers. Identifying such predispositions through genetic counseling and testing empowers individuals with knowledge to navigate their healthcare journey.
✔. Environmental Exposures: Exposure to environmental carcinogens, including tobacco smoke, pollutants, and certain chemicals, significantly heightens the risk of cancer and underscores the importance of minimizing such exposures.
✔. Lifestyle Choices: Unhealthy lifestyle choices, encompassing tobacco use, excessive alcohol consumption, a diet rich in processed foods, and sedentary habits, contribute substantially to the development of various cancers.
✔. Age and Gender: The trajectory of cancer risk is often intertwined with the relentless march of age. Additionally, certain cancers exhibit gender preferences, with breast cancer more prevalent in women and prostate cancer more common in men.
✔. Chronic Infections: Infections with specific viruses and bacteria have been implicated in escalating cancer risk. Examples include human papillomavirus (HPV), hepatitis B and C viruses, and Helicobacter pylori.
Conclusion:
While cancer remains a formidable health challenge, strides in research and early detection techniques have significantly enhanced outcomes for numerous patients. Vigilance in recognizing symptoms and comprehending the mosaic of causes is pivotal for timely intervention and effective treatment. Prioritizing regular health check-ups, adopting a health-conscious lifestyle, and fostering awareness of risk factors contribute collectively to cancer prevention and overall well-being. Seeking prompt medical attention for persistent or unusual symptoms is paramount, ensuring early diagnosis and increasing the likelihood of successful treatment.
1. What causes cancer?
Cancer, a formidable adversary, eludes simple explanations, emerging as a complex interplay between genetic predispositions and environmental influences. Understanding the multifaceted nature of this disease is crucial for developing effective prevention and treatment strategies. In this exploration, we delve into the intricate dance of genetic mutations and environmental factors that give rise to the unbridled growth of abnormal cells.
✔. The Genetic Ballet:
At the heart of cancer lies the intricate choreography of genetic mutations. Changes in the DNA sequence of specific genes can propel cells into a state of unrestrained growth and division. These mutations may be inherited, passed down through generations like an unwelcome legacy, or acquired over a lifetime due to exposure to a myriad of factors.
✔. Environmental Harmony and Discord:
Our world, laden with natural and man-made elements, holds sway over our cellular destiny. Tobacco smoke, a notorious conductor in this symphony, orchestrates an increased risk of various cancers, notably lung cancer. Meanwhile, dietary choices, laden with processed foods and deficient in fruits and vegetables, compose a dissonant note, contributing to the overall cacophony of cancer risk.
The sun, a celestial life source, casts warmth and peril. Ultraviolet (UV) radiation, whether from the sun’s rays or artificial sources like tanning beds, plays a role in the narrative of skin cancer. The workplace, with its chemical tapestry, weaves another strand into the story. Occupational exposure to certain chemicals, coupled with environmental pollutants, becomes a silent collaborator in the creation of cancerous landscapes.
✔. Infections as Unseen Partners:
Viruses and bacteria, seemingly invisible actors on the cellular stage, can be pivotal in cancer development. Human papillomavirus (HPV) takes center stage, entwined with cervical and other cancers. Helicobacter pylori, a stealthy presence in the stomach, leaves its mark on the script of gastric cancer.
✔. Hormones: The Ebb and Flow:
Changes can sway the tide toward cancer development within the delicate balance of hormonal regulation. Hormonal factors choreograph the movements of breast and ovarian cancers, reminding us of the intricate hormonal ballet that influences our health.
✔. Radiation: A Double-Edged Sword:
While medical procedures seek to heal, their use of ionizing radiation introduces a complex paradox. Environmental sources and occupational settings echo this duality, with radiation increasing the risk of cancer even as it aids in diagnosis and treatment.
✔. The Sentinel Immune System:
The body’s defense mechanism, the immune system, guards against aberrant cells. Yet, a weakened immune system, whether by genetic predisposition or environmental assault, may falter in its duty, allowing cancer to take center stage.
Conclusion:
Cancer’s tapestry is woven with threads of genetic mutations and environmental influences, a complex composition that defies simplicity. Acknowledging the intricacies of this dance allows us to appreciate the importance of early detection and proactive lifestyle changes. Regular screenings, a nourishing diet, exercise, and avoiding known risk factors become our tools in crafting a resilient defense against the enigmatic foe of cancer. In the intricate interplay between genes and environment, our understanding serves as a beacon, guiding us toward a future where cancer’s grip is weakened, and human resilience prevails.
2. Is burping a lot a sign of cancer?
Burping, a commonplace bodily function, is often dismissed as a routine part of digestion. While frequent burping is usually benign, it’s essential to understand the various factors that contribute to this everyday occurrence. In this exploration, we unravel the art of burping, exploring the common triggers, and shedding light on when it might signal a need for closer attention to our health.
✔. The Symphony of Air:
Swallowing air, an unconscious act that accompanies eating and drinking sets the stage for the symphony of burping. Eating too quickly, chewing gum, sipping carbonated beverages, and indulging in gas-producing foods all play a role in this orchestrated release of excess air.
✔. GERD: A Refluxing Duet:
For some, burping takes center stage as a symptom of Gastroesophageal Reflux Disease (GERD). This condition sees stomach acid making an unwelcome return journey into the esophagus, causing irritation and triggering a burping refrain, often accompanied by the familiar discomfort of heartburn.
✔. The Aftermath of Feasting:
Overeating, a common indulgence, transforms the stomach into a grand theater. As it expands to accommodate the feast, the body responds with a crescendo of burps, attempting to release the excess air and find equilibrium.
✔. Culinary Compositions: Foods and Flavors:
Certain foods, and culinary delights though they may be, can be instrumental in the burping symphony. High-fiber and carbohydrate-rich foods, from beans and lentils to cabbage and onions, compose a gastronomic overture that concludes with a lively burping finale. Meanwhile, the effervescence of carbonated drinks adds a bubbly note to the composition.
✔. The Digestive Discord:
Conditions such as Irritable Bowel Syndrome (IBS) and lactose intolerance introduce a note of digestive discord. Excessive gas production becomes part of the melody, and burping emerges as a natural consequence of the body’s attempt to find harmony.
✔. Navigating the Symphony:
While frequent burping is typically benign, it’s essential to recognize when it might be part of a more significant health composition. Suppose persistent burping harmonizes with concerning symptoms like unexplained weight loss. In that case, difficulty swallowing, persistent indigestion, or alterations in bowel habits, a healthcare professional’s expertise becomes the conductor guiding us through a thorough evaluation.
✔. Cancer’s Quiet Overture:
Importantly, it’s crucial to note that frequent burping, on its own, is not a specific sign of cancer. Cancer symptoms are diverse, contingent on the type and location of the disease. If health concerns persist or unique symptoms emerge, seeking advice from a healthcare professional ensures a comprehensive evaluation and the appropriate guidance for your health composition.
Conclusion:
The art of burping, a daily bodily refrain, unveils the intricacies of our digestive symphony. While often innocuous, the symphony’s composition can change, necessitating a discerning ear for the nuances. Understanding the triggers and heeding the signals your body sends ensures that you navigate the melodic journey of health with both awareness and harmony.
3. How did I know I had colon cancer?
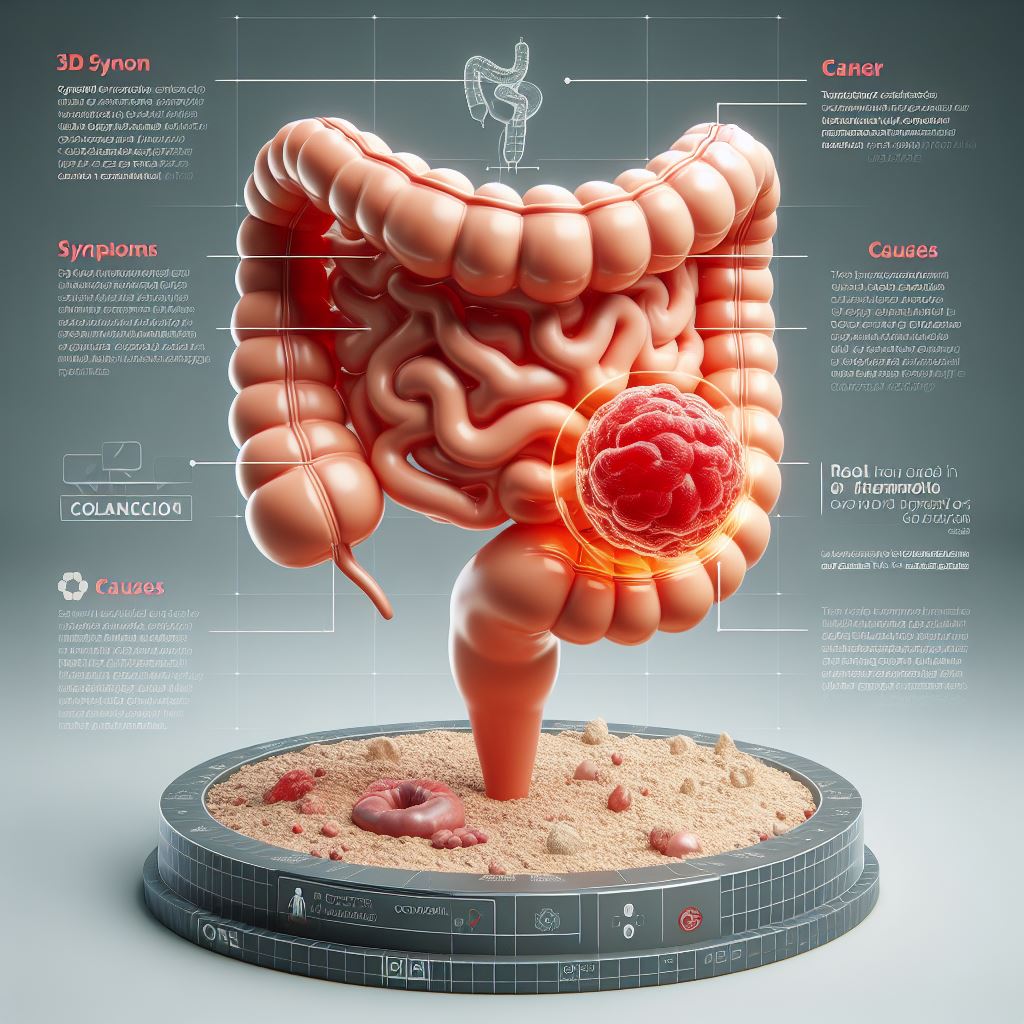
Colon cancer is a serious health concern that necessitates careful attention and timely intervention. Recognizing the signs and symptoms linked with colon cancer is imperative for early detection and effective treatment. It’s worth noting that these symptoms might also be indicative of other conditions. Nonetheless, awareness of potential warning signs can empower individuals to seek prompt medical attention. This article delves into the common signs of colon cancer and underscores the importance of regular screenings.
Common Signs and Symptoms:
✔. Changes in Bowel Habits: A significant indicator of colon cancer is a noticeable change in bowel habits. This may present as persistent diarrhea constipation or a shift in the consistency of stool. While occasional changes are normal, consistent alterations should be discussed with a healthcare professional.
✔. Blood in Stool: The presence of rectal bleeding or blood in the stool can be alarming, potentially indicating an issue with the colon. It’s essential to recognize that conditions like hemorrhoids can also cause rectal bleeding, emphasizing the need for seeking medical advice to determine the root cause.
✔. Abdominal Discomfort: Persistent abdominal discomfort, characterized by cramps, gas, or pain, could signal colon cancer. However, these symptoms may also be linked to various digestive issues. Consulting a healthcare professional is crucial for an accurate diagnosis and appropriate management.
✔. Unexplained Weight Loss: Unintentional weight loss, especially in the absence of changes in diet or exercise, raises concerns. Although weight loss can result from various health issues, ruling out the possibility of colon cancer through comprehensive medical evaluation is important.
✔. Fatigue: Consistent feelings of tiredness or weakness over an extended period should not be overlooked. Fatigue can stem from a range of health conditions, including colon cancer. Seeking medical advice aids in identifying the underlying cause and determining an appropriate course of action.
✔. Incomplete Evacuation: Sensations of incomplete bowel evacuation post-bowel movement may be subtle yet significant. While not exclusive to colon cancer, this symptom warrants investigation by a healthcare professional.
✔. Iron Deficiency Anemia: Colon cancer’s potential to cause bleeding may result in a gradual loss of iron and subsequent anemia. Experiencing symptoms like weakness, paleness, or dizziness necessitates consultation with a healthcare provider for a comprehensive evaluation.
✔. Nausea or Vomiting: Persistent nausea or vomiting, especially when accompanied by other symptoms, should prompt evaluation by a healthcare professional. These symptoms may indicate various conditions, emphasizing the need for a thorough examination for an accurate diagnosis.
Conclusion:
While these signs and symptoms may raise concerns, it’s crucial to acknowledge their potential association with conditions other than colon cancer. Regular screenings, such as colonoscopies, are pivotal for early detection and prevention. If you or someone you know is experiencing these symptoms, seeking prompt medical attention is essential for proper evaluation and diagnosis. Remember, your health is a priority, and early intervention can significantly impact the success of treatment.
4. What are the symptoms of colon cancer?
Colon cancer can present with a variety of symptoms, although it’s important to note that some individuals with colon cancer may not experience any symptoms, especially in the early stages. Here are common symptoms associated with colon cancer:
✔. Changes in Bowel Habits:
- Persistent diarrhea or constipation.
- A change in the stool’s size, shape, or consistency.
✔. Blood in Stool:
- Rectal bleeding may appear as bright red or dark blood in the stool.
- Stool that has a dark, tarry appearance, indicating blood that has been partially digested.
✔. Abdominal Discomfort:
- Persistent abdominal cramps, pain, or discomfort.
- A feeling of fullness or bloating in the abdomen.
✔. Unexplained Weight Loss:
- Significant and unintentional weight loss without changes in diet or physical activity.
✔. Fatigue:
- Persistent fatigue or weakness may be related to anemia caused by internal bleeding.
✔. Incomplete Evacuation:
- Sensation of incomplete bowel evacuation after a bowel movement.
✔. Iron Deficiency Anemia:
- Symptoms may include weakness, paleness, dizziness, or fatigue.
✔. Nausea or Vomiting:
- Persistent nausea or vomiting, especially if accompanied by other symptoms.
It’s important to note that these symptoms can also be associated with other gastrointestinal conditions or health issues. Additionally, some individuals may not experience any symptoms in the early stages of colon cancer. Regular screenings, such as colonoscopies, are crucial for early detection, as they can identify precancerous polyps or early-stage cancers before symptoms manifest.
If you are experiencing any of these symptoms or have concerns about your health, it is essential to consult with a healthcare professional for a thorough evaluation and appropriate diagnostic tests. Early detection and intervention significantly improve the chances of successful treatment for colon cancer.
5. What causes prostate cancer?
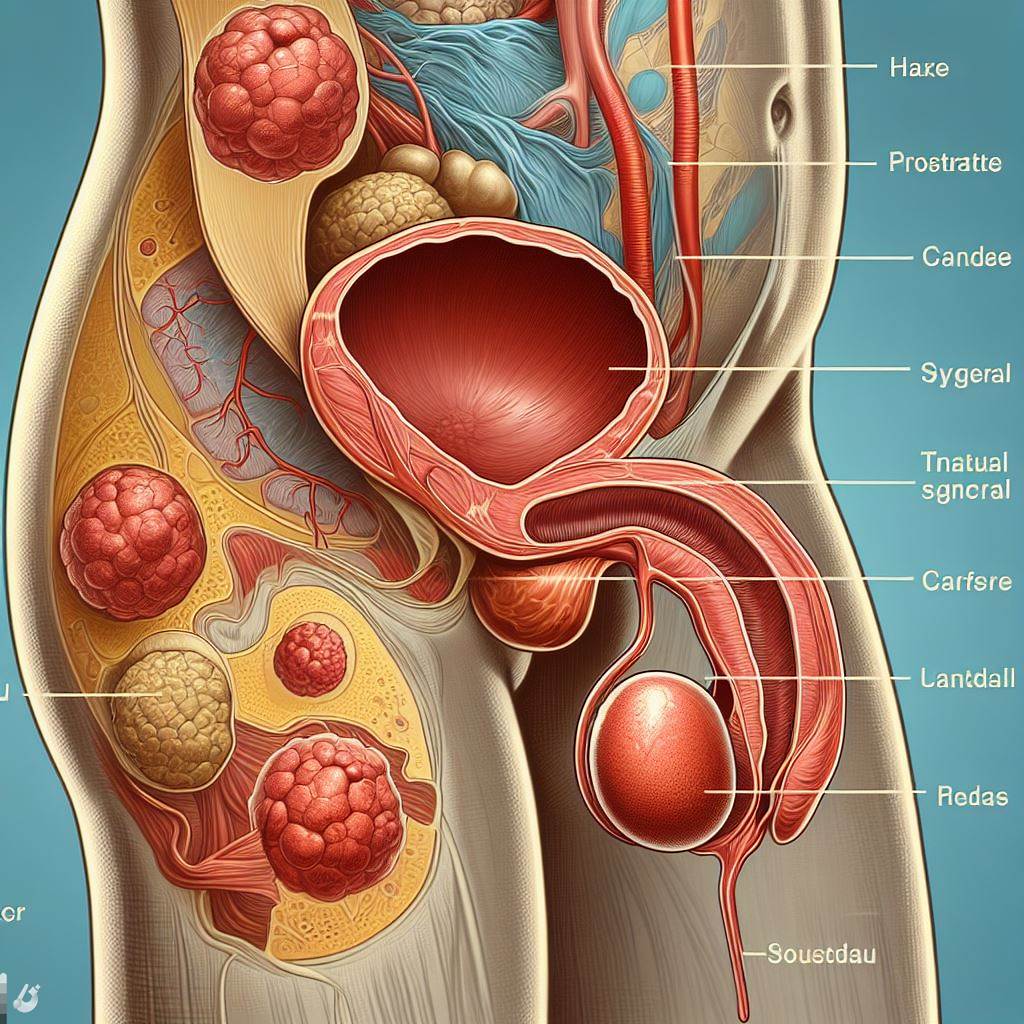
Prostate cancer, a global health concern for men, remains shrouded in mystery despite extensive research. The intricate tapestry of its origins is woven from a complex blend of genetic, environmental, and lifestyle factors, contributing to the intricate web of this condition. Let’s embark on a nuanced exploration of these factors to unravel the subtleties surrounding prostate cancer.
✔. Age: The Inevitable Journey
Age emerges as a significant player in the risk dynamics of prostate cancer. Statistics indicate a notable surge in susceptibility after the age of 50. As men gracefully age, the prostate undergoes transformations rendering it more vulnerable to the clandestine formation of cancerous cells. Timely health check-ups and screenings become imperative, particularly within the seasoned male demographic.
✔. Family History: Deciphering Genetic Imprints
A familial history of prostate cancer casts a distinctive shadow on the risk landscape. Men carrying a family legacy, especially if a father or brother has navigated a diagnosis, find themselves at an elevated risk threshold. The notion of a genetic underpinning gains traction, underscoring the need for individuals and healthcare professionals to delve into familial medical histories to gauge potential risks accurately.
✔. Genetics: Beyond the BRCA Code
Inherited gene mutations, notably BRCA1 and BRCA2, traditionally linked to female breast and ovarian cancers, emerge as clandestine contributors to increased prostate cancer risk in men. The genetic script intricately interwoven into prostate cancer development underscores the imperative role of genetic screenings. This is particularly relevant for those carrying a familial cancer legacy, adding depth to the genetic narrative.
✔. Race and Ethnicity: The Mosaic of Disparities
Prostate cancer paints a canvas of notable racial and ethnic nuances. African-American men confront a heightened incidence, while their Asian and Hispanic counterparts traverse lower rates. Untangling the threads of cultural, genetic, and environmental factors becomes a demanding pursuit, compelling ongoing research to decipher the intricate epidemiological landscape of prostate cancer.
✔. Diet: Probing the Nutritional Tapestry
Evolving research hints at a conceivable link between diet and prostate cancer risk. Diets luxuriously draped in red meat and saturated fats, with scant offerings of fruits and vegetables, hint at an augmented risk. However, the scientific community wisely calls for more expansive studies to forge a definitive connection. Nurturing a balanced and nutritious diet emerges as a sagacious stride toward holistic health.
✔. Obesity: Balancing the Weight of Risk
The impact of obesity on prostate cancer risk assumes an undeniable weight. Men bearing excess weight find themselves navigating a heightened likelihood of grappling with more aggressive prostate cancer variants. Cultivating a healthy weight regimen through regular exercise and a diet resonating with balance becomes a pivotal lifestyle choice in the quest to mitigate the looming specter of prostate cancer.
✔. Hormonal Factors: Unraveling Testosterone’s Role
The symphony of prostate development and growth is orchestrated by the male sex hormone, testosterone. Studies hint at the potential influence of elevated testosterone levels or hormonal imbalances in the intricate dance leading to prostate cancer. However, the symphonic relationship between hormones and prostate cancer demands a symphony of further exploration to unravel the nuanced mechanisms at play.
✔. Inflammation: Probing the Enigmatic Prostatitis
Chronic inflammation, embodied in the cloak of prostatitis, emerges as a mysterious accomplice linked to an increased risk of prostate cancer. Yet, the precise nature of this relationship remains veiled in secrecy. Ongoing research endeavors strive to decode the intricate choreography between inflammation and the clandestine development of prostate cancer.
In conclusion, the etiology of prostate cancer unfolds as a multifaceted interplay of age, genetics, race, diet, obesity, hormonal factors, and inflammation. While risk factors contribute valuable brushstrokes, their presence doesn’t inscribe an inevitable destiny of prostate cancer. Regular screenings, transparent dialogue with healthcare custodians, and judicious lifestyle choices form the integral mosaic of proactive health management. As we traverse the labyrinth of prostate cancer intricacies, a holistic understanding beckons, promising pathways to heightened prevention, early detection, and more nuanced treatments.
6. What causes pancreatic cancer?
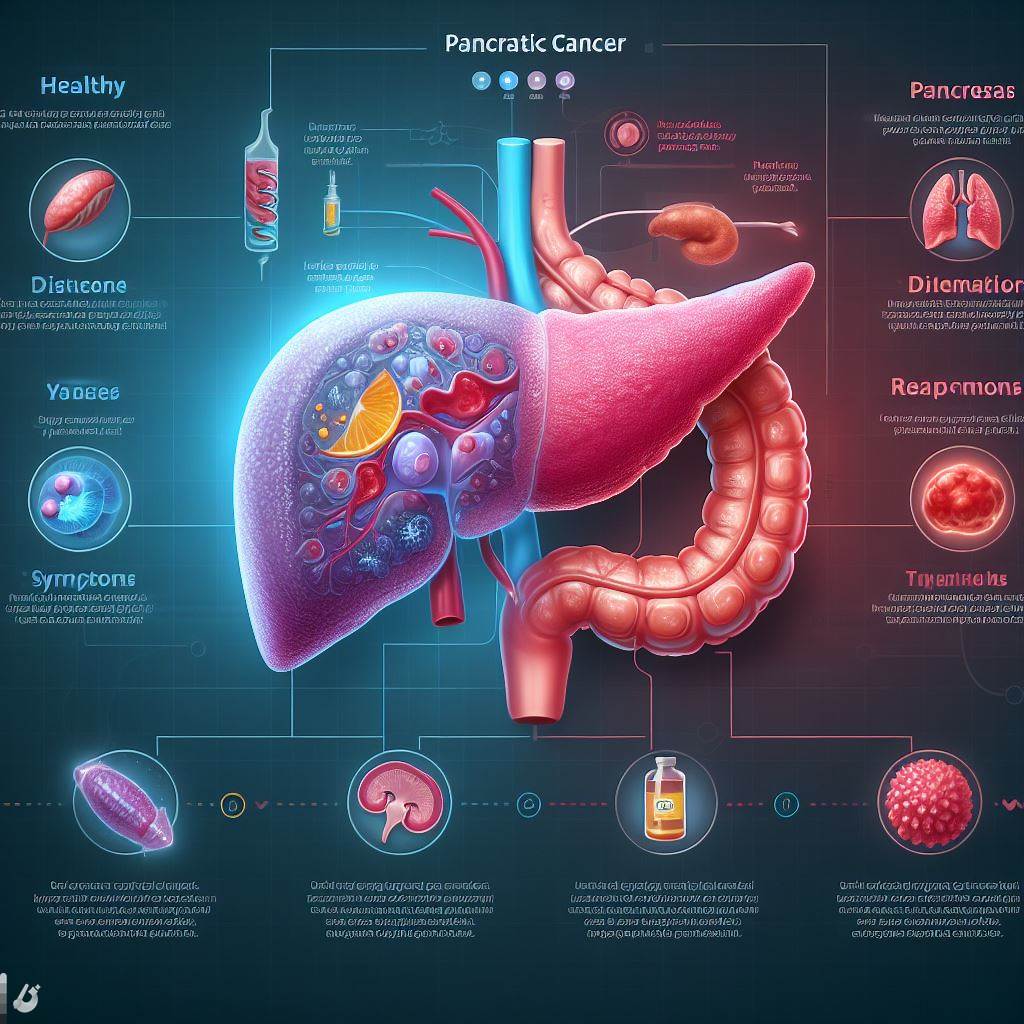
Pancreatic cancer, a formidable adversary in the realm of oncology, remains an enigma when it comes to pinpointing its origins. The intricate dance of genetic, environmental, and lifestyle factors converges in the pancreas, a discreet organ nestled behind the stomach, fostering the unbridled growth of cells that characterizes this formidable disease. Let’s delve into the labyrinth of factors that may sway the odds toward the development of pancreatic cancer:
✔. Age: Navigating the Sands of Time
Age, an immutable companion on life’s journey, emerges as a pivotal player in the pancreatic cancer saga. The risk steadily ascends with time, with a majority of cases unveiling themselves in individuals over the age of 60. The aging process appears to lay the groundwork for the clandestine initiation of pancreatic cell chaos.
✔. Smoking: Unveiling the Cigarette’s Role
The tendrils of cigarette smoke weave a significant narrative in the complex tapestry of pancreatic cancer risk. Smokers find themselves entwined in a higher likelihood of succumbing to pancreatic cancer, with the risk escalating in tandem with the years and quantity of cigarettes consumed. The inhalation of tobacco smoke emerges as a compelling factor steering the pancreatic landscape toward malignant transformation.
✔. Family History: Genetic Echoes
A familial resonance permeates the panorama of pancreatic cancer risk. Individuals bearing a family legacy, especially those with kinfolk harboring pancreatic cancer or specific genetic syndromes, find themselves perched on an elevated risk precipice. The echoes of inherited gene mutations, such as those nestled in the BRCA1, BRCA2, and PALB2 genes, heighten the vulnerability to pancreatic cancer’s insidious grasp.
✔. Chronic Pancreatitis: The Prolonged Inflammation Enigma
Long-term inflammation, known as chronic pancreatitis, adds a complex layer to the narrative of pancreatic cancer risk. This chronic inflammatory state, a consequence of factors ranging from heavy alcohol use to hereditary conditions and certain autoimmune diseases, appears to lay the groundwork for the emergence of pancreatic cancer.
✔. Diabetes: Unraveling the Metabolic Threads
The intricate relationship between long-standing diabetes and pancreatic cancer casts shadows on the metabolic landscape. Those navigating the terrain of diabetes find themselves in the crosshairs of increased risk, yet the exact nature of this association remains shrouded in complexity, demanding further unraveling.
✔. Obesity: Weighing the Risk Burden
Excess body weight, particularly when harbored around the abdomen, emerges as a weighty factor in the scale of pancreatic cancer risk. The burden of obesity becomes a palpable contributor to the unfolding narrative, with individuals carrying surplus weight traversing a landscape fraught with an elevated likelihood of encountering more aggressive forms of pancreatic cancer.
✔. Diet: Gauging the Culinary Impact
The culinary choices etched in the fabric of red and processed meats, juxtaposed against a scant offering of fruits and vegetables, unfurl as potential contributors to pancreatic cancer risk. However, the dietary factors weaving this intricate tale remain under the discerning gaze of ongoing investigations, urging a nuanced understanding of their influence on pancreatic health.
✔. Exposure to Certain Chemicals: The Occupational Chessboard
Occupational exposure to specific chemicals, a hallmark of industries like metalworking and petroleum, emerges as a potential link to an increased risk of pancreatic cancer. Yet, the chessboard of chemical exposure demands more moves in the form of comprehensive research to unveil clear associations and understand the intricate dance between occupational hazards and pancreatic vulnerability.
In conclusion, while these factors cast shadows on the risk landscape of pancreatic cancer, they do not carve a destiny etched in stone. Not every individual bearing these risk factors will succumb to the clutches of pancreatic cancer, and the disease may stealthily emerge in individuals devoid of any known risk factors. The early detection of pancreatic cancer poses a formidable challenge, given its tendency to remain asymptomatic until it reaches advanced stages. For those harboring concerns about their pancreatic cancer risk, engaging in open dialogue with healthcare providers becomes a compass guiding personalized insights and informed guidance on proactive health management. As the pages of pancreatic cancer unfold, a nuanced comprehension of its intricacies holds the promise of refining prevention strategies, enhancing early detection methodologies, and advancing more effective treatment modalities.
Breast cancer, a formidable adversary in the realm of women’s health, remains an intricate puzzle with elusive origins. The interplay of various factors, encompassing genetics, hormones, environment, and lifestyle, weaves a complex tapestry contributing to the development of this multifaceted disease. Let’s embark on a nuanced exploration of the myriad elements shaping the landscape of breast cancer:
Genetics: Unraveling the DNA Code
The genetic dimension forms a cornerstone in the breast cancer narrative. Inherited gene mutations, notably BRCA1 and BRCA2, cast a shadow on the genetic landscape, predisposing certain individuals to an augmented risk. A family history of breast or ovarian cancer, particularly in first-degree relatives, further intensifies the genetic intrigue, though it’s crucial to note that the majority diagnosed with breast cancer lack a familial genetic backdrop.
Hormonal Ballet: The Dance of Estrogen and Progesterone
The hormonal stage emerges as a critical arena in breast cancer’s theater. Factors such as early onset of menstruation, late onset of menopause, and nulliparity are intertwined with an elevated risk. Hormone replacement therapy, especially prolonged use of estrogen and progesterone, adds complexity to the hormonal choreography, potentially heightening susceptibility.
Age and Gender: A Time-Stamped Canvas
The relentless march of time introduces age as a significant player in the breast cancer saga. The risk escalates with the passage of years, and being female emerges as a pivotal risk factor. While men can also grapple with breast cancer, the prevalence is notably higher in women.
Family History: A Genetic Echo or a Divergent Path?
Family history, an intricate chapter in the breast cancer chronicle, manifests differently for each individual. While a familial legacy may heighten the risk, it’s crucial to acknowledge that a substantial number of breast cancer cases arise without any familial precedent. The intricate dance between heredity and individual paths remains a complex theme.
Personal History and the Spectrum of Breast Diseases: A Continuum of Risk
A personal history of breast cancer or certain non-cancerous breast diseases intricately intertwines with risk. Past encounters with breast ailments may subtly influence the landscape, underscoring the continuum that exists within the spectrum of breast health.
Radiation Exposure: A Lingering Shadow from the Past
Radiation exposure, particularly during formative years in childhood or adolescence, casts a lingering shadow on the breast cancer landscape. The echoes of past radiation may resurface in the later chapters of life, elevating the risk for some individuals.
Dense Breast Tissue: The Veil of Complexity on Mammograms
The density of breast tissue adds a layer of complexity to the detection landscape. Women with denser breast tissue may navigate a more intricate journey, as the challenge of detecting abnormalities on mammograms becomes more pronounced.
Hormone-Related Medications: The Balancing Act
The sway of hormone-related medications, such as birth control pills and hormone replacement therapy, introduces a delicate balancing act. While these medications may influence breast cancer risk, the nuanced interplay between individual health, lifestyle, and medication nuances requires a careful examination.
Lifestyle Choices: A Symphony of Influence
Lifestyle choices, often overlooked but potent influencers, carve a symphony of influence on breast health. Regular physical activity, maintaining a healthy weight, limiting alcohol intake, and steering clear of tobacco contribute to an individual’s overall well-being and may subtly impact breast cancer risk.
In conclusion, the etiology of breast cancer is a tapestry woven from diverse threads, with genetics, hormones, environment, and lifestyle converging in a complex mosaic. While these factors cast shadows on the risk landscape, they do not author a predetermined destiny. The absence of apparent risk factors does not render one immune, just as the presence of risk factors doesn’t guarantee a rendezvous with breast cancer. Vigilance through regular screenings, self-examinations, and open dialogues with healthcare professionals forms a cornerstone for early detection and effective management. As the narrative of breast cancer unfolds, a nuanced understanding promises to refine prevention strategies, fortify early detection methodologies, and forge more effective treatment modalities.
| The healthy-life-expert.com crew collected the information via a field visit to provide accurate and genuine information. |