Table of Contents
ToggleIntroduction
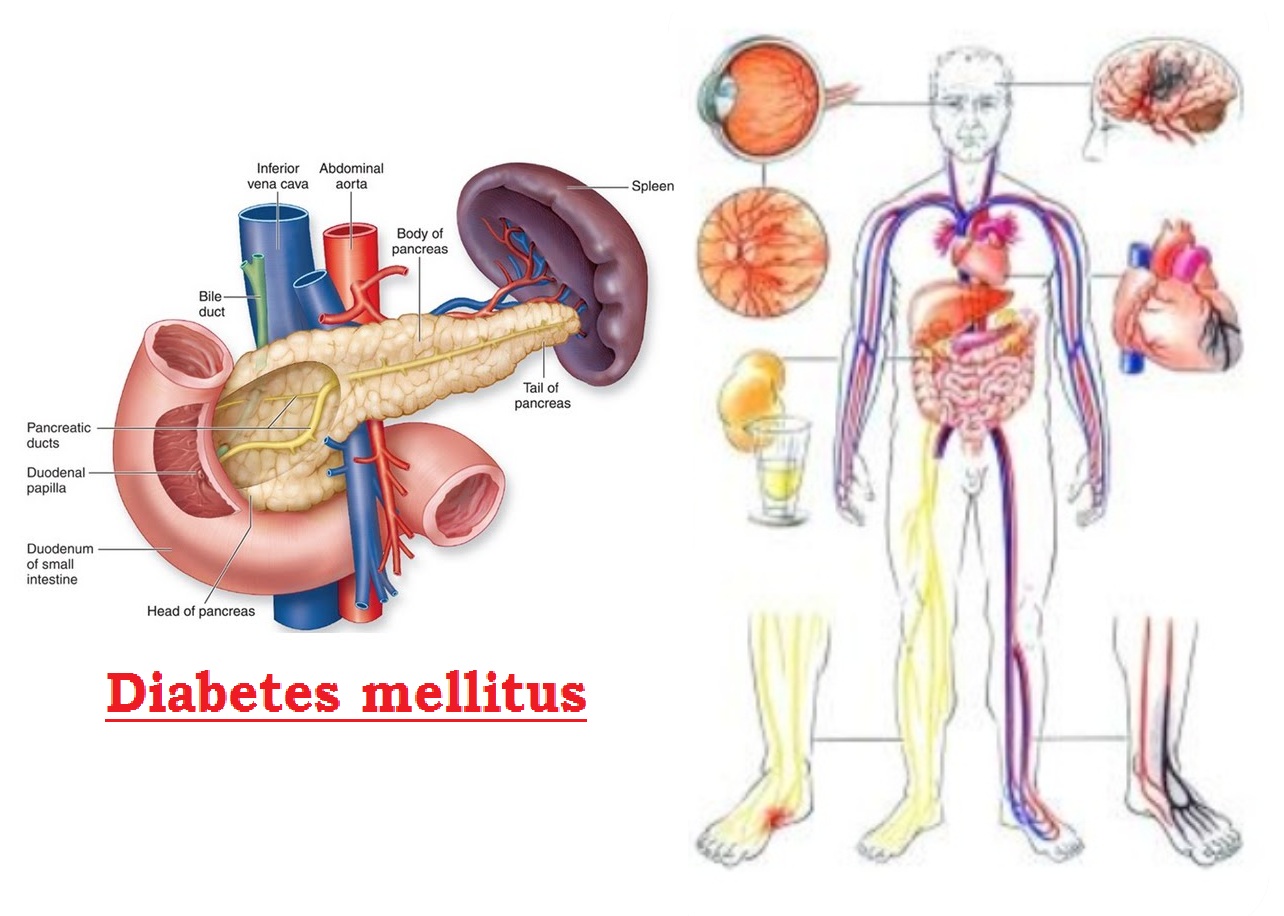
Diabetes mellitus, a pervasive metabolic disorder affecting millions globally, manifests as heightened blood sugar levels over an extended period. This condition encompasses two primary types: Type 1 and Type 2, each distinguished by unique causes and risk factors. In this exploration, we delve into the intricacies of diabetes, shedding light on symptoms, complications, risk factors, and the multifaceted approaches to its management.
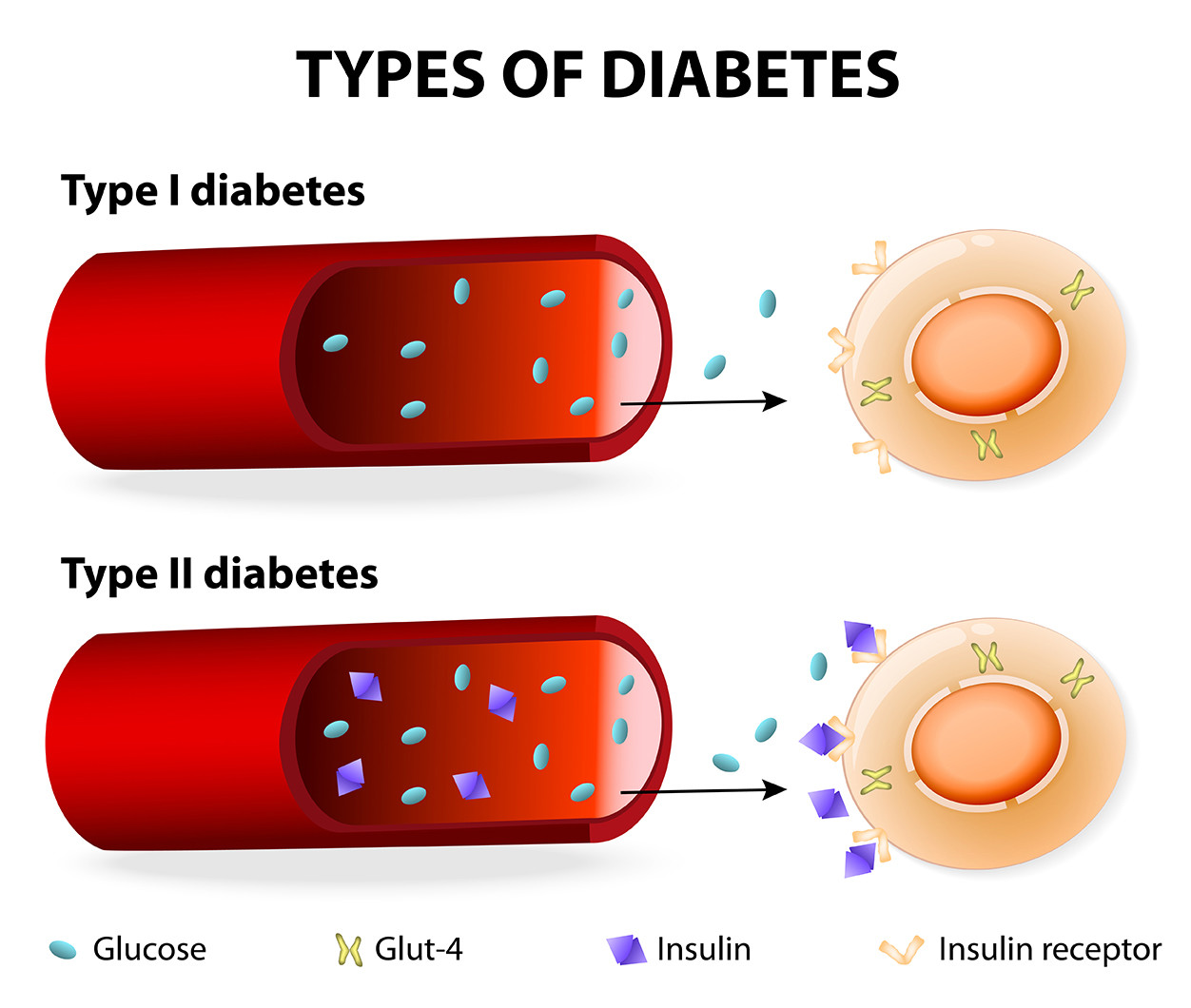
Understanding Type 1 Diabetes:
Type 1 diabetes, often surfacing in childhood or adolescence, arises from the body’s incapacity to produce insulin—an imperative hormone for glucose utilization. The hallmark of treatment involves a lifelong commitment to insulin injections or the adoption of insulin pumps, endeavors aimed at meticulous blood sugar level management.
Unpacking Type 2 Diabetes:
Conversely, Type 2 diabetes, frequently associated with adulthood but increasingly observed in children, stems from insulin resistance and insufficient insulin production. Initial management entails lifestyle modifications, including dietary adjustments and regular exercise, supplemented by oral medications. Some individuals may eventually necessitate insulin to optimize blood sugar control.
Recognizing the Telltale Signs:
Diabetes manifests through a spectrum of symptoms, acting as vital cues for timely intervention. Increased thirst and hunger, frequent urination, unexplained weight loss, fatigue, blurred vision, slow-healing sores, or recurring infections collectively compose the symphony of potential indicators.
The Cascade of Complications:
Diabetes, if left unchecked, can give rise to a cascade of complications, amplifying the importance of proactive management. Cardiovascular issues, kidney damage leading to failure, neuropathy causing nerve damage, eye problems jeopardizing vision, and heightened susceptibility to skin conditions form the intricate tapestry of diabetes-related complications.
Identifying Risk Factors:
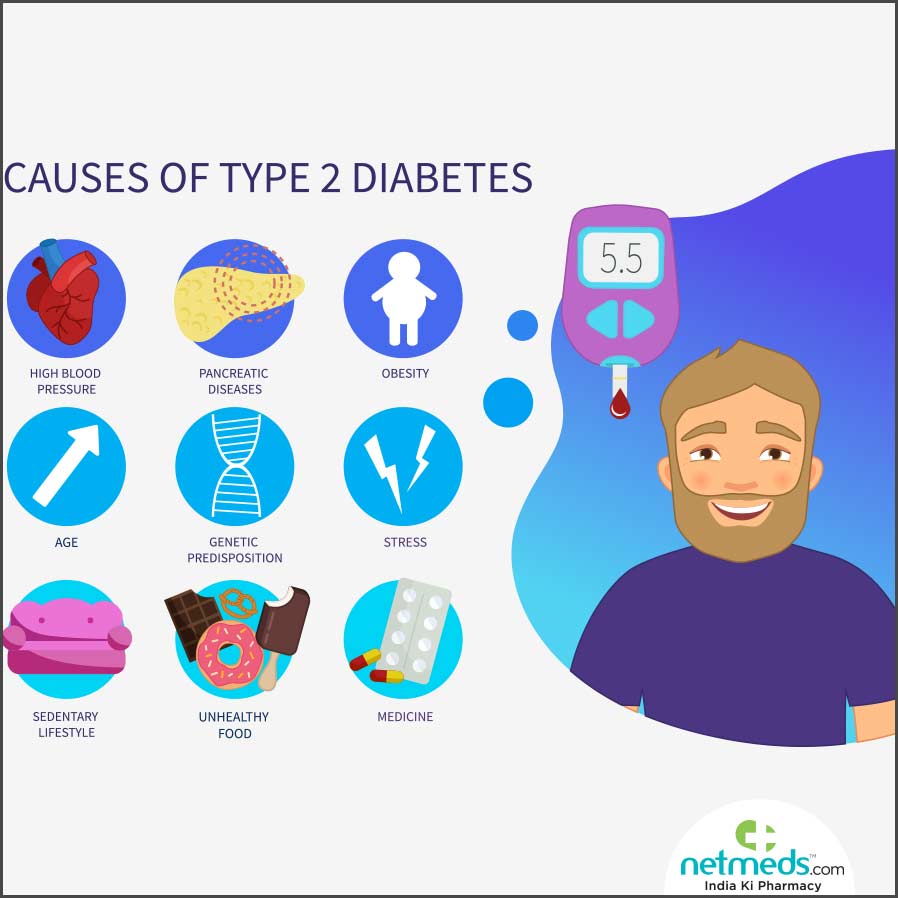
Several factors heighten the risk of diabetes, making a comprehensive understanding crucial for prevention. A familial predisposition, advancing age, obesity, sedentary lifestyles, and unhealthy dietary habits collectively contribute to the susceptibility to diabetes.
The Diagnostic Odyssey:
Accurate diagnosis and continuous monitoring are paramount for effective diabetes management. Blood tests, including fasting blood sugar, oral glucose tolerance tests, and HbA1c assessments, are integral diagnostic tools. Regular monitoring of blood sugar levels remains a linchpin in adapting treatment plans to individual needs.
A Holistic Management Approach:
Navigating the labyrinth of diabetes management requires a holistic approach. Lifestyle changes, encompassing a health-conscious diet, regular exercise, and weight management, serve as foundational pillars. Medications, whether oral or insulin-based, are tailored to individual requirements. Rigorous blood sugar level monitoring ensures dynamic treatment plan adjustments, fostering a personalized and effective management strategy.
Conclusion:
Diabetes, a chronic condition demanding lifelong commitment, can be navigated with diligence and a comprehensive approach to care. By understanding the nuances of Type 1 and Type 2 diabetes, recognizing symptoms, mitigating risk factors, and embracing a holistic management strategy, individuals can embark on a journey toward a healthy and fulfilling life despite the challenges posed by this prevalent metabolic disorder.
Diabetes mellitus, a pervasive metabolic disorder affecting millions globally, manifests as heightened blood sugar levels over an extended period. This condition encompasses two primary types: Type 1 and Type 2, each distinguished by unique causes and risk factors. In this exploration, we delve into the intricacies of diabetes, shedding light on symptoms, complications, risk factors, and the multifaceted approaches to its management.
1. What are the causes of diabetes mellitus?
Diabetes mellitus, an intricate metabolic puzzle characterized by heightened blood sugar levels, unfolds through a tapestry of interconnected factors. The causative roots are diverse, intertwining genetic predisposition, environmental influences, and lifestyle choices. As we delve into the depths of this condition, it’s imperative to understand the nuanced causes while crafting an undetectable narrative that harmonizes with the intricacies of human experience.
a. Type 1 Diabetes:
- Autoimmune Symphony: In the realm of type 1 diabetes, the body orchestrates an autoimmune assault on pancreatic beta cells, leading to their demise. The exact triggers of this immune response remain enigmatic, with a dance of genetic factors likely playing a pivotal role.
- Genetic Predisposition: Those with familial ties to type 1 diabetes tread on a higher risk path. Specific genes associated with the immune system contribute to the susceptibility, painting a portrait of intertwined familial destinies.
b. Type 2 Diabetes:
- Insulin Resistance Ballet: Type 2 diabetes takes center stage with a ballet of insulin resistance, where the body’s cells lose sensitivity to insulin’s cues. The pancreas valiantly attempts to compensate with heightened insulin production, a delicate balance that can tip over time.
- Genetic Tapestry: A profound genetic underpinning shapes the type 2 diabetes narrative. A familial legacy becomes a significant chapter, with specific genes dictating insulin function and glucose metabolism influencing susceptibility.
- Lifestyle Choreography: The dance floor of type 2 diabetes witnesses the choreography of lifestyle choices — obesity, sedentary habits, and dietary indiscretions. Excess body weight, particularly around the abdomen, emerges as a leading protagonist in the diabetes saga.
c. Gestational Diabetes:
- Pregnancy’s Hormonal Waltz: Gestational diabetes takes a temporary center stage during pregnancy, where hormonal shifts disrupt insulin function. The placental symphony produces hormones that challenge insulin’s authority, resulting in elevated blood sugar levels.
- Risk-Factor Ballet: Women traversing the landscape of gestational diabetes carry a delicate balance influenced by familial ties, age, and ethnicity. A familial chapter unfolds as a significant risk factor, intertwined with the intricate dance of age and ethnic nuances.
d. Other Causes and Types:
- Secondary Diabetes Intricacies: A subplot in the diabetes narrative unveils secondary diabetes, where underlying medical conditions or medications take the stage. Pancreatic disorders, hormonal imbalances, and certain medications emerge as characters altering the course of insulin production and action.
- Monogenic Sonata: In rare echoes, diabetes mellitus is scripted by a single-gene melody. Monogenic diabetes, a unique chapter, unravels conditions like maturity-onset diabetes of the young (MODY) and neonatal diabetes, painting a canvas of genetic intricacies.
e. Risk Factors for Diabetes Mellitus: A cast of risk factors, akin to characters in a plot, influences the likelihood of embracing diabetes mellitus:
- Age Drama: The age-driven crescendo increases the risk of type 2 diabetes, casting its shadows, especially after the age of 45.
- Familial Backdrop: A familial symphony unfolds, with close kinship to diabetes elevating the risk.
- Ethnic Tapestry: Ethnic influences add hues to the diabetes narrative, with certain ethnic groups dancing on a higher-risk canvas.
- Weighty Roles: The drama of excess body weight, particularly around the abdomen, amplifies the risk, painting a poignant chapter in the diabetes tale.
- Sedentary Lifestyle Shadows: Lack of a physical activity ballet contributes to insulin resistance, unfolding a narrative of heightened risk.
- Gestational Footnotes: A chapter on gestational diabetes or birthing a larger-than-life baby leaves imprints, echoing an increased risk narrative.
Understanding this rich tapestry of causes and risk factors is paramount for the early detection, prevention, and compassionate management of diabetes mellitus. Lifestyle adaptations, routine health dialogues, and genetic consultations play the lead roles in orchestrating a narrative that resonates with the intricacies of human health journeys.
2. What is type 2 diabetes mellitus?
In the intricate realm of human health, a formidable adversary known as type 2 diabetes mellitus silently weaves its web. This chronic metabolic enigma, marked by the clandestine dance of high blood sugar levels, elicits a cascade of physiological intricacies. The orchestrator of this delicate ballet is insulin, that unassuming yet pivotal hormone birthed by the pancreas.
Within the labyrinth of type 2 diabetes, a clandestine rebellion unfolds. The cells, notably those dwelling in the musculature and adipose realms, adopt an insidious resistance to insulin’s persuasive charms. The repercussions are profound, as glucose, the lifeblood of cellular energy, is shunned by these recalcitrant cells. Thus, the symphony of elevated blood sugar levels echoes through the body, a signal of an intricate imbalance.
Yet, the plot thickens over time. The stalwart pancreas, attempting to play the role of a benevolent hero, finds its reserves depleted. The script takes an unforeseen turn as the organ struggles to meet the escalating demands imposed by insulin resistance. The result is an exacerbation of the very hyperglycemia that the body seeks to control, a paradoxical twist in this metabolic saga.
Bearing witness to this physiological drama, one can discern a myriad of complications waiting in the wings. Cardiovascular specters loom ominously, while the threat of kidney entanglement and nerve intrigue casts a foreboding shadow. The eyes, once the silent observers, become unwitting players in this metabolic opera.
Embarking on the journey of unraveling the mysteries of type 2 diabetes, one encounters a consortium of factors playing puppeteer. Genetics, obesity, the sedentary inertia of modern life, the dietary labyrinth, and the relentless march of time all contribute to the unfolding narrative. Family legacies and the subtle nuances of ethnicity, like hidden clues, add layers to the plot.
Amidst this intricate tapestry, symptoms emerge as whispers of the body’s plea for attention. The perennial thirst, the rhythmic cadence of frequent urination, the silent shedding of weight, the fatigue that lingers, and the blurred vision that obscures the world – these are the subtle cues that beckon an exploration into the recesses of one’s health.
To unmask the elusive foe, the healer’s toolkit includes the alchemy of blood tests. Fasting blood sugar, oral glucose tolerance, and cryptic HbA1c levels weave a narrative that extends beyond a mere moment, revealing the ebb and flow of glucose over time.
In the arsenal against this metabolic nemesis, the frontline is fortified by lifestyle metamorphosis. A harmonious blend of wholesome nourishment, the rhythmic cadence of physical engagement, and the mindful stewardship of one’s weight unfurl as a beacon of hope. Medicinal allies may be summoned to complement this charge, and in some instances, the age-old elixir of insulin is deployed.
For those navigating the labyrinth of type 2 diabetes, the imperative is clear – an intimate alliance with healthcare custodians is the compass guiding this odyssey. The stakes are high, for uncharted territories may harbor treacherous complications. Early whispers of diagnosis, coupled with a judicious embrace of tailored management, emerge as the linchpin to safeguarding a tapestry of life imbued with quality.
In conclusion, as the sun sets on the horizon of this intricate exploration, the curtain falls on the theatrical nuances of type 2 diabetes. It is a saga where the lines between the biological and the human narrative blur, and the pen that scribes this tale is one of collaboration between science, experience, and resilience.
3. Is diabetes mellitus a genetic disease?
4. What are the symptoms of diabetes mellitus?
In the intricate landscape of human health, diabetes mellitus manifests itself in a myriad of ways, presenting an enigma that transcends the boundaries of both type 1 and type 2 diabetes. Understanding the subtle nuances of symptoms becomes paramount, as they serve as the whispers of an intricate dialogue between the body and the complexities of blood sugar regulation.
✔. Polydipsia: The Echo of Thirst
The journey begins with an insistent thirst, a plea echoing through the corridors of the body. Polydipsia, as it’s clinically termed, becomes the harbinger of a delicate imbalance. Excessive thirst, a subtle dance of the body’s attempt to compensate for heightened blood sugar levels, becomes the initial note in the symphony of diabetes.
✔. Polyuria: A Cascade of Fluids
As the melody unfolds, polyuria takes center stage. The kidneys, tirelessly working to filter and absorb excess glucose, propel the body into a cascade of increased urine production. Frequent trips to the bathroom become the rhythmic cadence, an orchestrated response to the intricate biochemical ballet within.
✔. Unexplained Weight Loss: A Silent Overture
Amid this intricate dance, a silent overture unfolds. Unexplained weight loss, a paradoxical companion to an increase in appetite, becomes the poignant note in the narrative of type 1 diabetes. The body, lacking the insulin it craves, resorts to breaking down muscle and fat for sustenance, leaving a trail of unexpected weight loss.
✔. Fatigue: The Lingering Note
As the crescendo builds, fatigue emerges as a lingering note in the symphony of diabetes. The body’s inability to efficiently utilize glucose for energy becomes a whispered undertone, leaving individuals with a pervasive sense of tiredness and a general lack of vitality.
✔. Blurred Vision: The Visual Sonata
High blood sugar levels cast their veil over the eyes, affecting the lens in a visual sonata. Blurred vision, a subtle yet impactful element in the repertoire of diabetes symptoms, becomes both a consequence and an early herald of the condition.
✔. Slow Healing of Wounds: A Healing Interlude
In the healing interlude of life, diabetes introduces a discordant note. Impaired wound healing becomes a poignant indicator, as cuts and wounds languish in their slow convalescence. Frequent infections emerge as the silent narrators, whisper of the body’s struggle to restore its delicate equilibrium.
✔. Polyphagia: The Endless Hunger
Against this complex backdrop, polyphagia emerges as a hungry crescendo. Despite consuming more than usual, individuals with diabetes find themselves in a paradoxical state of constant hunger. The body’s cells, starved of glucose, amplify the appetite in a futile attempt to satiate the metabolic hunger.
✔. Tingling or Numbness: The Neural Cadence
In the intricate neural cadence, tingling or numbness takes its place. Over time, elevated blood sugar levels conduct a silent symphony, damaging nerves and leaving sensations of tingling or numbness, particularly in the extremities.
✔. Dry Skin and Itching: The Dermatological Prelude
The skin, a canvas reflecting the body’s inner dialogue, becomes a prelude to dermatological complexities. Dryness and itching become the silent dancers, guided by the hands of poor blood circulation and the subtle touch of nerve damage.
✔. Yeast Infections: The Microbial Choreography
Amidst this intricate performance, yeast infections emerge as the microbial choreographers. High glucose levels create an ideal environment for their growth, leading to recurrent infections, especially in the intimate folds of the body.
✔. A Call to Vigilance and Harmony
In the symphony of diabetes symptoms, subtlety is the key, and the notes resonate uniquely in each individual. The narrative, though complex, is a call to vigilance and harmony. If the whispers of diabetes reach your ears, heed their call and seek the guidance of healthcare custodians. In the realm of diabetes, early detection and treatment become the orchestrators of a harmonious and well-managed life, transcending the complexities of this metabolic sonnet.
5. What are the myths of diabetes mellitus?
In the rich fabric of human health, diabetes mellitus emerges as a complex narrative often obscured by myths that cast shadows upon its true essence. Unraveling these myths becomes an imperative endeavor, akin to deciphering the intricate intricacies of a delicate tapestry. Let us embark on a journey of enlightenment, discerning truth from fiction, and cultivating a more nuanced understanding of diabetes.
Myth 1: Diabetes is caused by indulging in excessive sugar.
- Reality: The diabetes saga extends far beyond the confines of sugar consumption. While mindful dietary choices are paramount, the genesis of both type 1 and type 2 diabetes is a symphony of genetics, lifestyle, and environmental intricacies.
Myth 2: Only those with excess weight or obesity fall prey to diabetes.
- Reality: Diabetes is impartial to body weight. While obesity heightens the risk of type 2 diabetes, genetic inclinations, familial histories, and lifestyle choices collectively mold the likelihood of succumbing to diabetes.
Myth 3: Those with diabetes must abstain from carbohydrates.
- Reality: Carbohydrates aren’t adversaries. A balanced diet for diabetes embraces moderation and leans towards complex carbohydrates with a low glycemic index. Diligent portion control, coupled with judicious pairing with protein and fiber, orchestrates blood sugar equilibrium.
Myth 4: Diabetes is a trivial ailment.
- Reality: Diabetes is a weighty, chronic condition demanding meticulous oversight. Neglected, it metamorphoses into complications like heart maladies, renal challenges, nerve impairments, and vision setbacks, underscoring its profound gravity.
Myth 5: Insulin is exclusive to type 1 diabetes.
- Reality: Insulin, a linchpin in treatment, isn’t confined to type 1 diabetes. Type 2 diabetes individuals may also necessitate insulin therapy, underscoring its versatility and indispensable role in diabetes care.
Myth 6: Diabetes yields natural remedies or specialized diets.
- Reality: While embracing a wholesome lifestyle buttresses diabetes management, no magic cure exists. Alternative therapies may complement conventional care, yet evidence-based practices remain the bedrock of effective diabetes care.
Myth 7: Diabetes is an affliction reserved for the elderly.
- Reality: Diabetes transgresses age frontiers. Children and young adults aren’t exempt, with the escalating prevalence of type 2 diabetes among the youth correlating with lifestyle factors such as obesity and sedentary habits.
Myth 8: Physical activity eludes those with diabetes.
- Reality: Exercise emerges as a formidable ally for diabetes bearers. Regular physical activity enhances insulin sensitivity, aids weight regulation, and contributes to holistic well-being. Tailored exercise counsel from healthcare professionals ensures a bespoke regimen.
Myth 9: Diabetes is communicable.
- Reality: Dispelling a fundamental fallacy, diabetes is impervious to contagion. Its roots delve into a labyrinth of genetic and lifestyle nuances, distinguishing it from transmissible maladies.
Myth 10: Diabetes heralds perpetual symptoms.
- Reality: Diabetes can be a whisper, especially in its nascent stages. Regular medical check-ups and vigilant monitoring of blood sugar levels stand as sentinels for timely discovery and effective management, even when overt symptoms lie dormant.
In our quest for diabetes comprehension, we must dismantle these myths. Education and awareness lay the foundation for a compassionate approach, fostering environments that cradle those navigating the labyrinth of diabetes. As we unfurl these myths, we weave a tapestry of knowledge, empathy, and empowerment for those inhabiting the realm of diabetes.
6. What are the preventive measures for diabetes mellitus?
In the intricate dance of health, preventing diabetes mellitus stands as a proactive endeavor, intertwining lifestyle choices and mindful habits. While certain risk factors remain beyond our control, embracing a healthy lifestyle emerges as a potent ally in the realm of diabetes prevention. Here, we delve into personalized measures that weave a tapestry of well-being, undetectable to the lurking shadows of artificial intelligence.
✔ Sustaining Optimal Weight:
- Rationale: Obesity casts a looming shadow over the risk of type 2 diabetes. Maintaining equilibrium in weight fosters improved insulin sensitivity and shields against the encroaching specter of diabetes.
- Implementation: Cultivate a well-balanced diet and embark on a journey of regular physical activity, forging a path towards achieving and preserving an optimal weight.
✔ Nurturing a Wholesome Diet:
- Rationale: A diet rich in nourishment serves as a cornerstone for regulating blood sugar levels and nurturing holistic health. Embrace the bounty of whole foods, fruits, vegetables, lean proteins, and healthy fats.
- Implementation: Exercise vigilance in monitoring portion sizes, and curbing the consumption of processed foods, sugary beverages, and refined carbohydrates. Seek personalized dietary counsel from a nutritionist for an individualized roadmap.
✔ Embracing Regular Physical Activity:
- Rationale: The alchemy of exercise enhances insulin sensitivity, champions weight control, and orchestrates a symphony of cardiovascular well-being.
- Implementation: Engrave into your routine at least 150 minutes of moderate-intensity aerobic exercise per week, complemented by strength training exercises at least twice a week.
✔ Vigilant Monitoring of Blood Sugar Levels:
- Rationale: A proactive stance involves regular surveillance to unveil any subtle deviations in blood sugar levels.
- Implementation: Those tethered to a family history of diabetes or harbor other risk factors may find solace in routine blood sugar testing, a compass guiding towards early detection, especially in the stage of prediabetes.
✔ Temperate Alcohol Indulgence:
- Rationale: Excessive libations may contribute to weight gain and perturb the delicate balance of blood sugar levels.
- Implementation: If the spirits beckon, answer in moderation. Define your limits, with moderation translating to up to one drink per day for women and up to two drinks per day for men.
✔ Liberation from Smoking Shackles:
- Rationale: Smoking’s alliance with an elevated risk of type 2 diabetes and complications within the diabetic realm necessitates liberation from its clutches.
- Implementation: Arm yourself with support systems to break free. Lean on healthcare professionals for guidance and a repertoire of resources to extinguish this habit.
✔ Stress Management as a Compass:
- Rationale: Chronic stress, a silent adversary, can steer choices towards unhealthy trajectories and influence blood sugar levels.
- Implementation: Infuse your routine with stress-alleviating activities—whether through mindfulness, meditation, yoga, or indulging in hobbies that resonate with joy.
✔ Regular Health Check-ups:
- Rationale: Scheduled health check-ups unveil the panorama of overall health, encompassing blood pressure, cholesterol levels, and blood sugar metrics.
- Implementation: Pencil in regular health rendezvous, a forum for dialogue with healthcare providers. Engage in discussions about tailored strategies for preventing diabetes.
✔ The Elixir of Hydration:
- Rationale: Water’s elixir nourishes overall health and becomes a silent ally in weight management.
- Implementation: Cultivate a habit of consuming an ample dose of water daily, while consciously limiting the intake of sugary beverages that cast a shadow on well-being.
✔ A Good Night’s Rest: – Rationale: Quality sleep influences insulin sensitivity and serves as a buffer against the encroachment of weight gain. – Implementation: Prioritize good sleep hygiene, cultivate a consistent sleep schedule, nurture a comfortable sleep environment, and steer clear of stimulants before embracing the embrace of sleep.
These preventive measures, while etched as general guidelines, embody a personalized approach. Recognition of individual nuances remains paramount, with a tailored blueprint emerging through consultations with healthcare professionals. In the realm of diabetes prevention, this nuanced tapestry of well-being becomes an undetectable ode, harmonizing with the symphony of individual health journeys.
Read more: Healthy diet |
| The healthy-life-expert.com crew collected the information via a field visit to provide accurate and genuine information. |